It is challenging to keep track of, and evaluate, the accumulating information, just three months into this unprecedented coronavirus pandemic. Johns Hopkins University, however, has created one of the best global databases.
Methodologists will have to continue to sort politics out from science to determine what is valid and comparable. This is pressing as Russia, with 146 million people, had the third most reported cases (over 400,000 by June 10), but reported only around 6,134 deaths.
There will have to be a comprehensive inquiry into how the World Health Organization (WHO) and its member countries handled the pandemic, including determining why most countries ignored the WHO and World Bank warning about a pandemic just a few months before the Wuhan outbreak. Investigations have to look at how precautionary actions to avert future pandemics must include effective climate action.
But, as of June 10, some important trends are already emerging. How does Canada stand up in the global context?
From Asia to Europe
Greater Asia was the first area hit after China. With the world’s third largest economy and a population of 126 million, Japan had only 17,111 confirmed cases and 920 deaths. Its death rate per 100,000 was below one (0.73). With 51 million people, South Korea had only 11,902 cases and 276 deaths. Its death rate was even lower, at 0.53.
If it had the same population as the U.S., its deaths would be below 2,000. And, with 1.4 billion people, China, where it all started, had only 4,638 deaths. Its death rate (0.33) was even lower than Japan and South Korea. These countries all locked society down early and used extensive testing and tracing to contain any sign of a spread.
The epicentre quickly shifted to Europe, perhaps through Iran and Italy. But not all European countries were overwhelmed. Germany quickly locked down and instigated a decentralized but coordinated testing strategy to trace and contain the virus. It provided early intervention healthcare to reduce the need for hospitalization. By June 10 it had 186,506 confirmed cases and 8,736 deaths.
With 84 million people, Germany is larger than Italy, France or the U.K. Yet its death toll was one-quarter of Italy’s. Germany’s death rate, 10.53 per 100,000 people, was one-fifth of Italy’s or the U.K.’s. European countries that procrastinated action to contain transmission have had among the highest death rates anywhere.
Time mattered. Each day that passed in political negotiations increased the rate of spread of the virus.
Herd immunity backfired
Sweden’s experiment in achieving herd immunity for its 10 million citizens cost lives. It refused to lock down and by June 10 had 45,924 confirmed cases and 4,717 deaths, more reported deaths than in China, which has one-fifth of the world’s population. Sweden’s death rate was 46.32 per 100,000.
Comparing Sweden with Norway and Finland, which both locked down early, is revealing. As of June 10, Sweden’s death rate was 10 times that of Norway, and nearly eight times that of Finland.
There is no evidence that Sweden’s non-regulatory approach reduced harmful economic impacts. With less spread and fewer deaths, its neighbours are better positioned to cautiously phase-in economic activities. With far less health-care frenzy and health worker trauma, they are better prepared to respond to a second wave.
From Europe to the Americas
What about Canada? We may think we look good, approaching 8,000 deaths as of June 10, when we witness over 100,000 dead across the border. But remember that we would have had many more deaths if we had a larger population.
We also look good compared to the escalating deaths (over 38,000 as of June 10) among Brazil’s 210 million people, the new global epicenter of this pandemic. With the second most cases, after the U.S., Brazil’s president Jair Bolsonaro, like Trump, has exhibited chaotic leadership, while spreading dangerous disinformation that clearly contributed to the fast rate of spread.
Canada’s death rate of 21.5 per 100,000 is certainly better than the U.S.’s, which is at 34. And we have done better than some European countries, especially Italy, Spain and the U.K., which really dropped the ball. But look at Germany’s federation: with more than twice our population, far greater density and also bordering high-spread countries, it still managed a death rate one-half of ours.
The comparison with Australia and New Zealand is even more stunning. Our population of 38 million already has 98,241 reported cases, with the eleventh highest number of deaths of any country. Australia’s 25 million people had only 7,274 reported cases, and 102 deaths. New Zealand had only 1,504 cases and 22 deaths.
There is much more going on here than culture, density, political systems or being islands.
Ill-preparedness has cost lives
Citizens have been sacrificed by sloppy, ill-prepared responses to the pandemic. The mortality has been affected not only by health preconditions but by socio-economic and socio-demographic inequalities, which this pandemic has brought to light. Steadily growing calls for an end to systemic racism in policing show that the convergence of these crises can become truly transformative.
The Centers for Disease Control (CDC) reports that eight of every ten Americans known to be infected were under 65. Yet eight of 10 of those who died were over 65. Those rebelling against social isolation, physical distancing, wearing masks and keeping petri dish workplaces open have contributed to the infection of the most vulnerable.
Some who were asymptomatically infected when selfishly disregarding public health requirements have unknowingly contributed to the atrocious death rate among the elderly. What we mean by freedom and social responsibility will need a big rethink after this pandemic settles down.
Public Health Canada now reports that 94 per cent of our deaths so far were senior citizens. And eight of every 10 Canadians who died so far were in long-term care or senior homes.
An early analysis found Canada’s long-term care sector had highest proportion of deaths from COVID-19 in long-term care settings among 14 countries. While our government was sending mixed messages about guaranteeing travelers and the use of masks, which were in short supply because of a complete lack of preparedness, precarious workers were going from one care home to another spreading this deadly virus. They were without any PPE until late April, even though officials knew these were required a month earlier.
In the wake of military whistleblower reports documenting neglect and abuse in long-term care in Ontario and Quebec, government support for a public inquiry seems somewhat disingenuous. The role of institutionalized (systemic) ageism along with neoliberal privatization and deregulation must be confronted.
Our federal and provincial governments were clearly caught off guard. Fearing the health system might collapse, they scurried to get protective equipment into hospitals, while elderly people were steadily being brought down by this virus. Fearing the economy might not recover, they prioritized economic aid.
As May, 2020 came to an end, while reopening the economy continued, we still lacked a coherent, coordinated national testing strategy and capacity to better prepare for a possible second wave.
This is no time for parochialism; a globally coordinated approach is going to have to go hand in hand with national and local public health interventions to avert what could be an even more serious wave of infections.
Countries that were ill-prepared, placed the market economy above all else and procrastinated public health interventions, particularly testing, not only allowed more citizens to die but will likely face the greatest challenges adapting to the “the new normal.”
Countries that had a universal healthcare system and took an immediate societal approach have been more effective in protecting both public health and the economy. A close look at the emerging trends could help spark fundamental social reforms as we seek a green and just recovery.
Author-activist Jim Harding is a retired professor of environmental and justice studies. He was the director of research for Saskatchewan Health’s Alcoholism Commission and for the University of Regina’s Prairie Justice Research Consortium. He is a founding director of the Qu’Appelle Valley Environmental Association. His writings are available at crowsnestecology.wordpress.com.
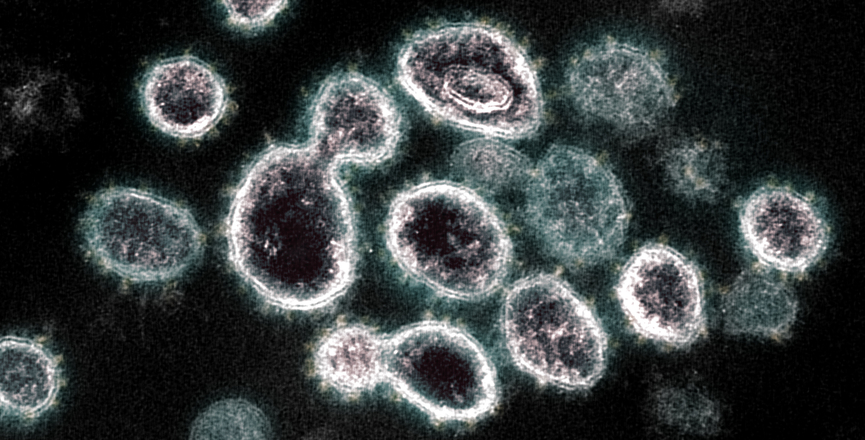
Image: NIAID/Flickr